Corneal grafting, also known as corneal transplantation, is a surgical procedure where a damaged or diseased cornea is replaced by donor corneal tissue from a recently deceased person. Eye banks collect healthy corneas from decedents – a careful history is taken to ensure that the donor had no known diseases which might affect the viability of the donor cornea – and these are then used by ophthalmologists (eye surgeons) in corneal graft surgery. Corneal transplants are fairly common operations – there are about 1000 performed in Australia each year – and the success rate is high (although this will vary depending on the indication for grafting). The probability of rejection is less than that of other transplants because the cornea has no blood supply.
The most common indication for corneal graft surgery in Australia is keratoconus, with over 30% of grafts performed for this reason. Other indications include bullous keratopathy, failed previous corneal grafts, corneal dystrophies and herpetic eye disease. The success rate for all corneal transplants – where ‘success’ is defined as graft survival after 5 years – is about 75%. Note that the success rate (as mentioned above) will depend on the indication for grafting and is very much related to the pre-operative condition of the host cornea. For example, corneal transplants for keratoconus are almost 100% successful due to the fact that this condition does not usually involve the peripheral cornea.
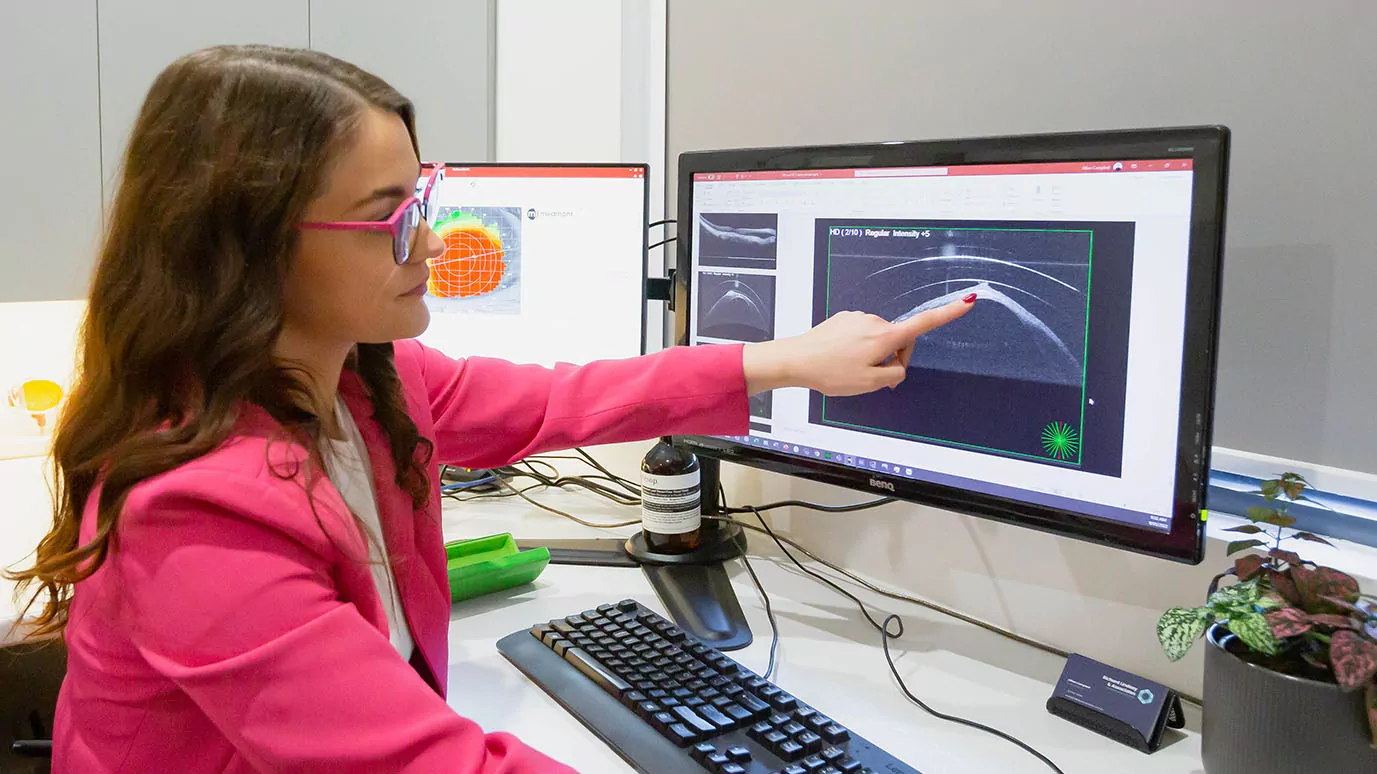
Penetrating keratoplasty (PK) is the most common form of corneal graft surgery. In this procedure the whole thickness of the cornea (including the corneal endothelium) is replaced by donor tissue. The corneal endothelium is the most posteriorly located structure of the cornea and is critical for the normal health and functioning of the cornea. During the corneal graft surgery, the surgeon will fasten the donor cornea to the host cornea either by use of a running suture or multiple interrupted sutures. These sutures will generally stay in place for about 1 to 2 years. Up until about 15 years ago, over 90% of corneal transplants in Australia were PK. With the development of newer forms of corneal transplantation (see below), only about 70% of corneal grafts are now the full thickness PK.
Deep anterior lamellar keratoplasty (DALK) involves removal of only partial corneal thickness and can be considered when the recipient’s corneal endothelium is relatively healthy (and not affected by the disease or condition that has necessitated the corneal graft). Unlike PK, in which endothelial cell viability of the donor cornea is critical to graft success, donor endothelium is not a consideration in DALK and by retaining the host’s own healthy endothelium, the risk of corneal graft rejection is greatly reduced. Note that if the patient’s own endothelium cannot be preserved during surgery, this procedure is easily converted to a PK without the need to reschedule surgery.
Endothelial transplants such as Descemet’s stripping automated endothelial keratoplasty (DSAEK) and Descemet’s Membrane Endothelial Keratoplasty (DMEK) are used to treat conditions affecting primarily the corneal endothelium such as Fuchs endothelial dystrophy and bullous keratopathy. Both DSAEK and DMEK remove Descemet’s membrane and endothelium. DMEK adds only a new Descemet’s membrane and endothelium. DSAEK also adds a new Descement’s membrane and endothelium, but also with a small layer of donor stroma as well. Endothelial transplants avoid the need for large surgical wounds, plus they minimize distortion that results from corneal graft astigmatism and provide a more rapid visual recovery than PK for certain conditions.
Once a patient is fully recovered from a corneal transplant and all the corneal graft sutures have been removed, about 10% of corneal graft patients will require no refractive correction, about 60% will be required to wear spectacles and approximately 30% will need to be fitted with contact lenses (usually of the rigid type) due to the presence of post-graft irregular astigmatism in the donor cornea. Wearing contact lenses does slightly increase the risk of corneal graft rejection. However, due to the advances in contact lens technology over the last 20 years, most corneal graft patients who are required to wear contact lenses generally do so without any major problems.